This study of California nurse practitioners (NPs) and certified nurse-midwives (CNMs) was conducted in early 2017. In November 2016, there were 20,337 NPs living in California, of whom 569 also were CNMs (“dual certified”). Another 582 people had CNM-only certification. Surveys were mailed to 2,500 NPs and CNMs, and the response rate was 64% of the eligible population, producing data from 1,588 NPs and CNMs. All analyses were weighted to ensure the results represent the total population of NPs and CNMs with California licenses.
Key Findings:
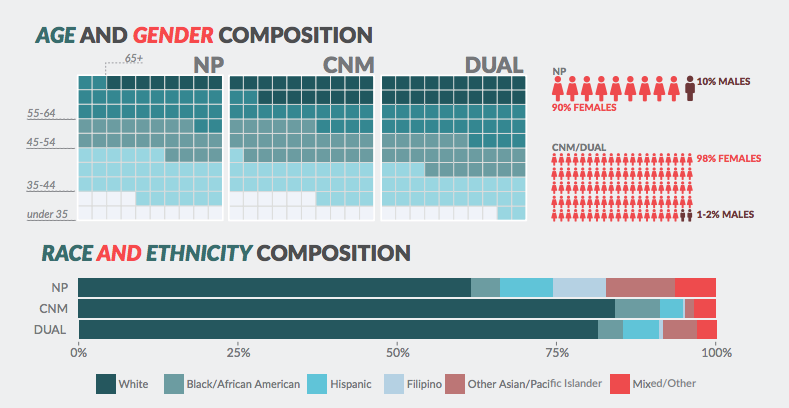
- The NP and CNM workforce is less diverse than the RN workforce as a whole. Men make up only 10.1% of NPs, and nearly no men hold a certificate as a nurse midwife. Over 60% of NPs and 80% of CNMs are white. The registered nurse workforce of California is becoming increasingly diverse, which provides an opportunity to recruit these diverse RNs into advanced practice
- There has been a notable influx of younger NPs into the workforce, with the largest age group being 35 to 44 years old (32.3%).
- At the time of the survey, 77.1% of all NPs and CNMs were working in positions that required their advanced practice certificates. Employment rates were higher for NPs (77.2%) than CNMs (70%), likely due to CNMs’ average older age.
- Around 84% of NPs reported that they were nearly always able to practice to the fullest extent of their legal scope of practice, and over 72% of CNMs reported that they work to the full extent of their scope of practice.
- More than 38% of NPs have a panel of patients they manage over time, but only 31.3% are recognized as a primary care provider by private insurance plans.
- When asked to rate their satisfaction with their work and careers, 82% of NPs and 92% of CNMs working as APRNs reported being “satisfied” or “very satisfied” with their APRN career.
- Among NPs and CNMs not working in advanced practice, more than 30% are retired. A large share of NPs and CNMs indicating a lack of jobs in desired clinical specialties, types of facilities, and geographic locations were a barrier to employment.
- In comments received from survey respondents, one of the most common themes was that of unmet potential. Whether through restrictive scope of practice or the failure of administrators and collaborators to use APRNs as primary care providers, the medical community is not taking advantage of the rich and extensive APRN training and experience. Many APRNs report that healthcare providers and physicians do not understand what an APRN can do.
